- Today
- Holidays
- Birthdays
- Reminders
- Cities
- Atlanta
- Austin
- Baltimore
- Berwyn
- Beverly Hills
- Birmingham
- Boston
- Brooklyn
- Buffalo
- Charlotte
- Chicago
- Cincinnati
- Cleveland
- Columbus
- Dallas
- Denver
- Detroit
- Fort Worth
- Houston
- Indianapolis
- Knoxville
- Las Vegas
- Los Angeles
- Louisville
- Madison
- Memphis
- Miami
- Milwaukee
- Minneapolis
- Nashville
- New Orleans
- New York
- Omaha
- Orlando
- Philadelphia
- Phoenix
- Pittsburgh
- Portland
- Raleigh
- Richmond
- Rutherford
- Sacramento
- Salt Lake City
- San Antonio
- San Diego
- San Francisco
- San Jose
- Seattle
- Tampa
- Tucson
- Washington
Research Reveals Molecular Cascade Behind Alzheimer's Disease
Baylor College of Medicine study uses fruit flies to identify key genes that drive neurodegeneration and those that may protect against it.
Published on Feb. 18, 2026
Got story updates? Submit your updates here. ›
A study published in Molecular Psychiatry has uncovered a path of cause-effect molecular events that can lead to Alzheimer's disease (AD). Researchers at Baylor College of Medicine, the Duncan Neurological Research Institute at Texas Children's Hospital, and collaborating institutions used a cross-species approach, integrating postmortem human brain gene expression analyses with laboratory fruit fly studies, to better understand how typical Alzheimer's brain changes, such as amyloid plaques and tau tangles, can lead to neurodegeneration and cognitive decline.
Why it matters
The findings provide new insights into the molecular cascade behind Alzheimer's disease, pinpointing specific driver genes and pathways that could serve as potential therapeutic targets. The researchers' 'biphasic' model suggests that early disease stages involve an increase in synaptic genes that hyperactivate brain cells, while later stages see a reduction in these same genes as a protective response, though ultimately too late to prevent further brain function deterioration.
The details
The researchers studied 344 genes whose expression was altered in human brains with Alzheimer's disease, including immune response genes with increased expression that promoted neurodegeneration when similarly activated in fruit flies. Surprisingly, silencing synaptic regulation genes in flies - which show reduced activity in Alzheimer's brains - actually protected brain cells from death, suggesting this may be a compensatory response to damaging brain cell hyperactivity.
- The study was published in the journal Molecular Psychiatry in February 2026.
The players
Dr. Joshua Shulman
Professor of neurology, neuroscience and molecular and human genetics at Baylor College of Medicine, and an investigator and co-director of the Duncan Neurological Research Institute.
Baylor College of Medicine
The institution where the lead researcher, Dr. Joshua Shulman, is a professor and investigator.
Duncan Neurological Research Institute
The research institute at Texas Children's Hospital where Dr. Joshua Shulman is an investigator and co-director.
Accelerating Medicines Partnership (AMP)-AD
The target discovery consortium that analyzed about 2,000 postmortem brain tissue samples and identified 30 AD-associated gene expression networks.
Emory University
The institution where researchers Nicholas T. Seyfried and Allan I. Levey are affiliated.
What they’re saying
“One important way to investigate the molecular cascade leading to cognitive decline is to study brain gene expression changes from individuals with Alzheimer's disease when compared with those from healthy brains.”
— Dr. Joshua Shulman, Professor of neurology, neuroscience and molecular and human genetics at Baylor College of Medicine, and an investigator and co-director of the Duncan Neurological Research Institute (Molecular Psychiatry)
“Our new understanding of the molecular cascade and gene expression networks causing Alzheimer's disease pinpoints specific driver genes and pathways worthy of further study as potential therapeutic targets.”
— Dr. Joshua Shulman, Professor of neurology, neuroscience and molecular and human genetics at Baylor College of Medicine, and an investigator and co-director of the Duncan Neurological Research Institute (Molecular Psychiatry)
What’s next
The researchers plan to continue studying the specific driver genes and pathways identified in this study to further explore their potential as therapeutic targets for Alzheimer's disease.
The takeaway
This cross-species research approach, integrating human brain data with fruit fly studies, has provided valuable insights into the molecular mechanisms underlying Alzheimer's disease progression. The findings suggest a complex, biphasic process involving both detrimental and compensatory gene expression changes, which could inform the development of new treatments targeting the root causes of neurodegeneration.
Houston top stories
Houston events
Feb. 18, 2026
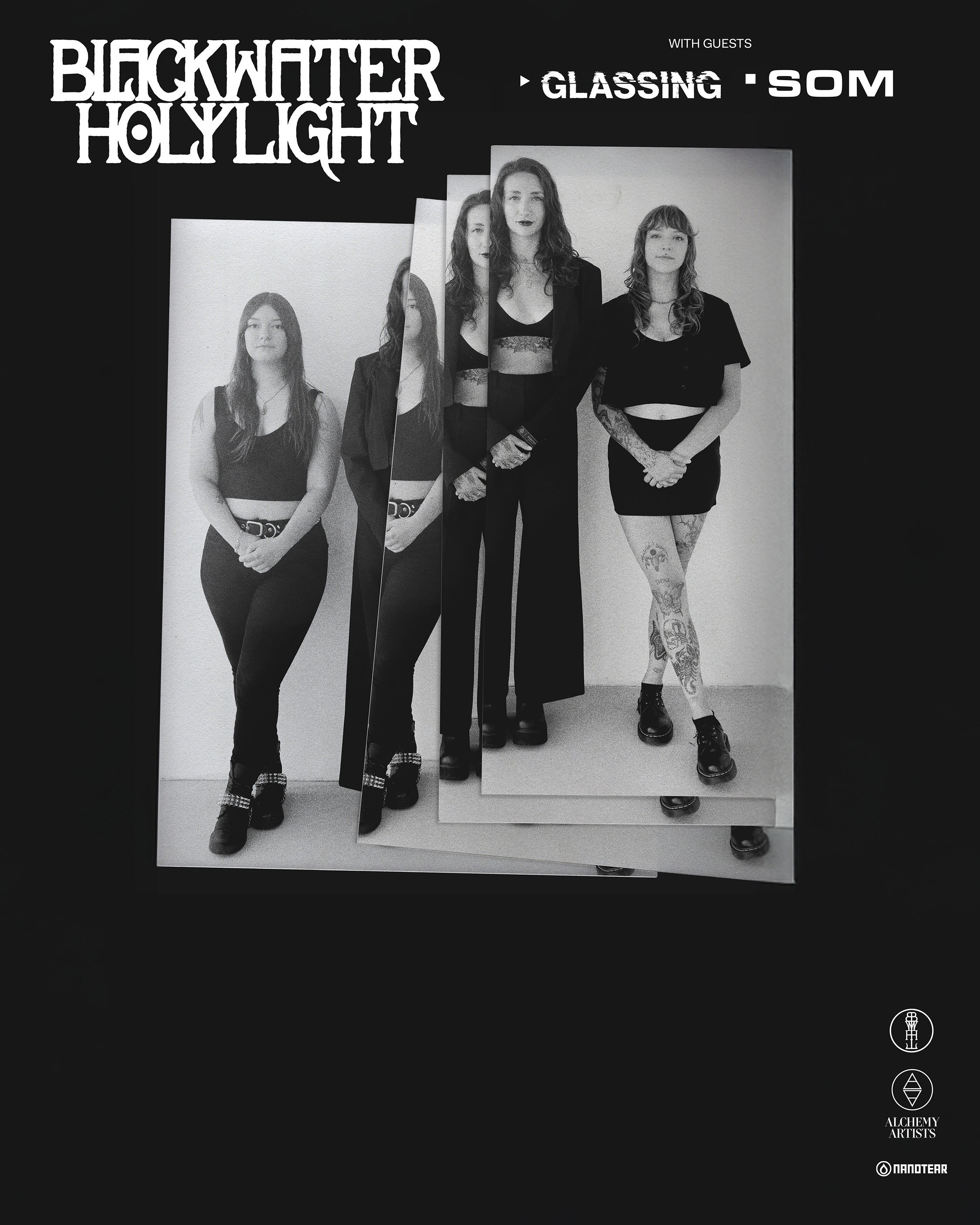
Blackwater HolylightFeb. 18, 2026
Peter McPoland: Big Lucky Tour